Endometriosis and Back Pain: When Pelvic Disease Shows Up in Your Spine & Hips
Endometriosis and back pain may happen when pelvic nerves or ligaments are involved. Learn symptoms that mimic sciatica, why it’s missed, and what to do. Check this out.
Dr. Smita Sinha
1/15/20264 min read
Lower back or hip pain is often blamed on posture, muscle strain, or spinal problems. Many people are told to rest, stretch, or attend physiotherapy. But for some women, the real cause lies much deeper. Endometriosis and back pain are more closely linked than many realise, and this connection is frequently overlooked.
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the womb. While it is commonly associated with painful periods, it can also affect structures far beyond the pelvis. When this happens, pain may be felt in the lower back, hips, groin, or even down the legs, leading to years of misdiagnosis and frustration.
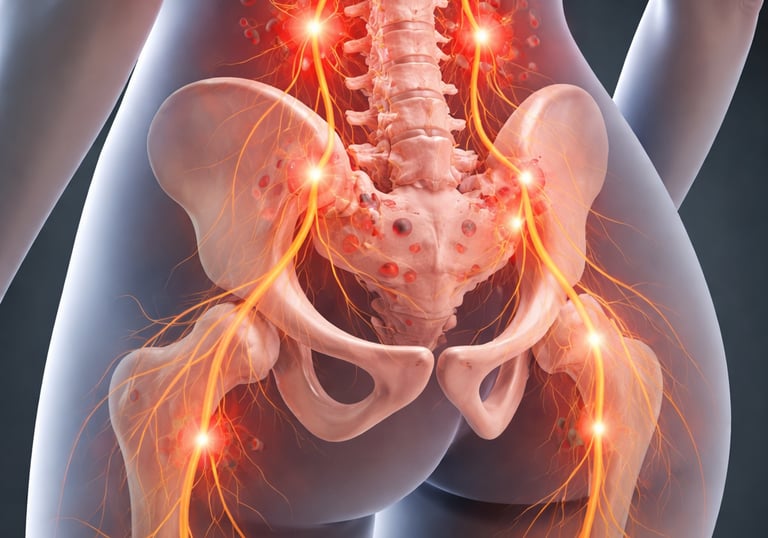
Why Endometriosis Can Cause Back or Hip Pain
Endometriosis does not only affect reproductive organs. It can involve ligaments, nerves, and tissues near the spine and pelvic joints. When these areas are affected, pain signals may be felt far from the uterus itself.
One common reason endometriosis and back pain are linked is the involvement of pelvic ligaments. Structures such as the uterosacral ligaments sit close to the lower spine and support the uterus. Endometriotic lesions in these ligaments can trigger deep, aching pain in the lower back, especially during menstruation.
Endometriosis can also irritate nearby nerves. When nerves are affected, pain may radiate to the hips, buttocks, or thighs. This nerve-related pain is sometimes mistaken for sciatica or disc problems, particularly when imaging of the spine appears normal.



When to Seek Help
If lower back or hip pain worsens around menstruation, keeps returning despite treatment, or is accompanied by other pelvic symptoms, further evaluation is important. Persistent pain should not be dismissed as normal or purely muscular.
Endometriosis and back pain can coexist silently for years. Seeking advice from a gynaecologist experienced in endometriosis can help uncover the root cause and guide appropriate care.


Management depends on the individual and the extent of disease. Treatment may involve hormonal therapy to reduce inflammation and suppress disease activity. Pain management strategies and lifestyle support can also play a role.
In cases where endometriosis is deeply infiltrating or affecting nerves and ligaments, surgery may be considered. Minimally invasive techniques aim to remove disease while preserving surrounding structures. Proper planning and specialist assessment are essential to achieve the best outcomes.
How Endometriosis-Related Back Pain Is Managed
Final Thoughts
Endometriosis does not always present as obvious pelvic pain. For many women, the first clue is unexplained back or hip pain that does not respond to conventional treatment. Understanding the link between endometriosis and back pain is an important step toward timely diagnosis and effective care.
If pain is affecting daily life, mobility, or well-being, listening to the body and seeking the right expertise can make a meaningful difference.
If symptoms persist or raise concern, consulting a gynaecologist experienced in endometriosis is recommended.
A common and frustrating experience for patients is being told that scans show nothing wrong. Standard X-rays or basic spinal imaging may not detect endometriosis at all. Even pelvic ultrasounds can miss deep or nerve-related disease.
This is why endometriosis and back pain often go unconnected. The pain is real, but the cause is hidden. In some cases, more detailed imaging such as MRI is needed to identify deep infiltrating endometriosis. Sometimes, the diagnosis is only confirmed during laparoscopy, which allows direct visualisation of affected tissues.
Back or hip pain linked to endometriosis often follows a pattern. Pain may worsen before or during menstruation. It may flare alongside other symptoms such as painful periods, pain during intercourse, or discomfort during bowel movements or urination.
Some women notice that physiotherapy, painkillers, or rest provide little or only temporary relief. When pain keeps returning despite appropriate musculoskeletal treatment, it is important to consider a gynaecological cause.
Recognising these patterns is key. Endometriosis and back pain are frequently connected when pain cycles with hormones rather than physical activity alone.


Ignoring persistent pain can have long-term consequences. Chronic pain can affect posture, muscle strength, and mobility over time. It can also take a toll on mental health, work performance, and overall quality of life.
Early assessment allows for a more accurate diagnosis and targeted treatment. Identifying endometriosis early can help prevent disease progression, reduce ongoing inflammation, and protect fertility in those who wish to conceive.





Why Scans Can Look Normal
Symptoms That Suggest a Gynaecological Cause
Why Early Assessment Matters
📞 Need Help?
To speak with a compassionate and experienced specialist, contact Dr. Smita, Consultant Gynaecologist at KPJ Selangor Specialist Hospital, Shah Alam.
💬 WhatsApp us at +60165833302 to book an appointment and get the personalised care you deserve.


Contact Us
Clinic: +60355433285
Whatsapp: +60165833302
Email: smitaobgyn@gmail.com


Why Us?
About Us
Services
Endometriosis
Robotic Surgery
Articles