Uterosacral Ligament Endometriosis: A Hidden Cause of Deep Pelvic Pain
Deep pelvic pain that persists despite treatment may be due to uterosacral ligament endometriosis. Learn symptoms, diagnosis, and when to see a specialist. Check this out!
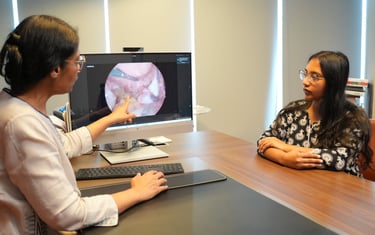
Dr. Smita Sinha
2/20/20264 min read
Persistent pelvic pain can be frustrating, especially when treatments do not seem to help or tests come back “normal.” For some women, the underlying cause may be uterosacral ligament endometriosis, a deep form of the disease that is often overlooked and difficult to diagnose.
Understanding this condition can help patients seek appropriate care earlier and avoid years of unnecessary suffering.
What Is Uterosacral Ligament Endometriosis?
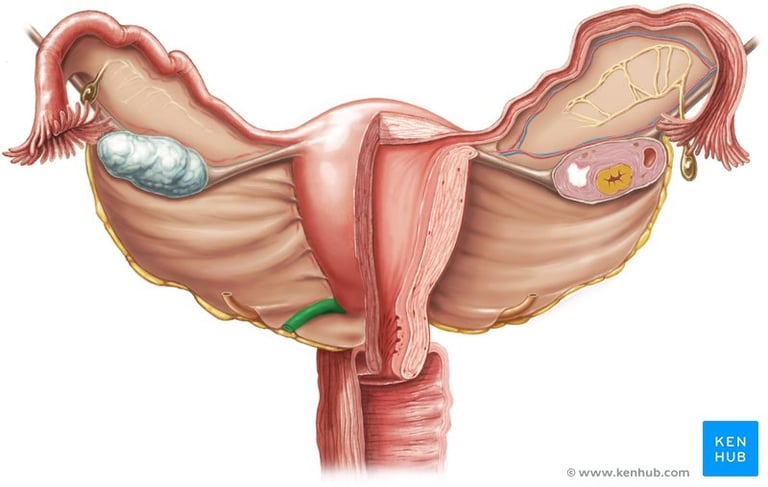
Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterus. While many people associate it with ovarian cysts or superficial lesions, the disease can also infiltrate deep structures in the pelvis.
The uterosacral ligaments are strong bands of tissue that connect the uterus to the sacrum (the lower spine). They sit deep in the pelvis, close to important structures such as the rectum, bladder, ureters, and pelvic nerves.
When endometriosis affects these ligaments, it is considered a form of deep infiltrating endometriosis. Because of its location, uterosacral ligament endometriosis often causes symptoms that go beyond typical period pain.


Why Specialist Care Matters
Deep infiltrating endometriosis often requires a multidisciplinary approach. Depending on the organs involved, the surgical team may include gynaecologists, colorectal surgeons, or urologists.
Specialised centres are better equipped to handle complex cases safely and thoroughly, reducing the risk of incomplete treatment or complications.
Management depends on symptom severity, fertility goals, and the extent of disease.
Medical Management
Hormonal therapies and pain management strategies may help control symptoms by suppressing menstrual cycles and reducing inflammation. These options are often used as first-line treatment.
However, medical therapy does not remove existing lesions.
Surgical Treatment
For women with significant symptoms or organ involvement, laparoscopic surgery may be recommended. During this procedure, surgeons carefully excise (cut out) endometriotic tissue while preserving surrounding structures.
In cases of uterosacral ligament endometriosis, surgery can be complex because of the proximity to nerves, ureters, and bowel. Some patients may require partial or complete resection of affected ligaments to achieve symptom relief.
When performed by experienced surgeons, excision surgery can significantly improve pain, quality of life, and fertility outcomes.
Treatment Options
When Should You Seek Medical Evaluation?
Persistent pelvic pain should not be ignored, especially if it interferes with daily life.
Consider consulting a gynaecologist if you experience:
Severe period pain that disrupts work or school
Deep pain during intercourse
Painful bowel movements during menstruation
Ongoing pelvic or lower back pain that does not improve
Symptoms that persist despite treatment
Early evaluation can prevent disease progression and reduce long-term complications.
The uterosacral ligaments are rich in nerve fibers and play a role in supporting pelvic organs. Inflammation, scarring, or nodules in this region can irritate nearby nerves and restrict organ movement.
This explains why women with uterosacral ligament endometriosis may experience:
Deep, severe menstrual pain
Chronic pelvic pain that persists throughout the month
Pain during or after sexual intercourse
Lower back or sacral pain
Pain during bowel movements, especially during menstruation
Because these symptoms overlap with other conditions such as irritable bowel syndrome, pelvic floor disorders, or musculoskeletal pain, diagnosis is often delayed.
Unlike large ovarian cysts, lesions on the uterosacral ligaments are not always visible on routine imaging. Standard ultrasounds may appear normal, especially if performed by providers without specific training in endometriosis mapping.
Additionally, pelvic examinations can be uncomfortable or inconclusive, and symptoms are sometimes dismissed as “normal period pain.”
As a result, women may live with uterosacral ligament endometriosis for years before receiving a definitive diagnosis.


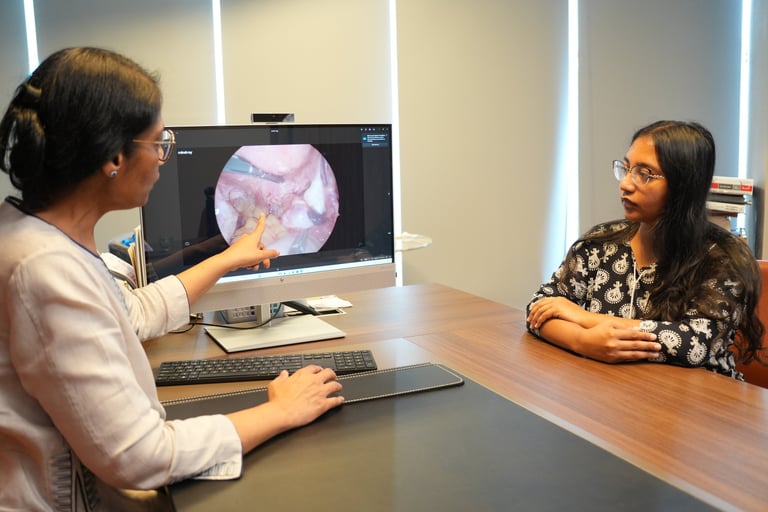
Accurate diagnosis typically requires a combination of clinical assessment and specialised imaging.
A gynaecologist experienced in endometriosis will carefully evaluate symptom patterns, particularly:
Pain that worsens around menstruation
Deep pelvic tenderness
Pain triggered by bowel or bladder activity
Persistent symptoms despite standard treatments
Advanced ultrasound techniques or MRI scans may detect deep lesions, scarring, or reduced mobility of pelvic organs. However, the most definitive diagnosis is often made during laparoscopy, a minimally invasive surgical procedure that allows direct visualisation of the pelvis.






Why This Area Causes Severe Symptoms
Why It Is Frequently Missed
How It Is Diagnosed
📞 Need Help?
To speak with a compassionate and experienced specialist, contact Dr. Smita, Consultant Gynaecologist at KPJ Selangor Specialist Hospital, Shah Alam.
💬 WhatsApp us at +60165833302 to book an appointment and get the personalised care you deserve.


Living With Uterosacral Ligament Endometriosis
Beyond physical symptoms, this condition can affect emotional wellbeing, relationships, and overall quality of life. Chronic pain is exhausting, and delayed diagnosis can be discouraging.
Support from healthcare providers, family, and patient communities plays an important role in coping and recovery.
The Takeaway
Uterosacral ligament endometriosis is a serious but treatable condition that often hides behind vague or misattributed symptoms. Because routine tests may miss it, awareness is essential for timely diagnosis.
Women experiencing deep, persistent pelvic pain deserve to be taken seriously. With proper evaluation and specialised care, effective treatment is possible, and many patients regain comfort, function, and confidence in their health.
If symptoms suggest endometriosis or are not responding to standard care, consulting a gynaecologist with expertise in endometriosis is an important next step.
Contact Us
Clinic: +60355433285
Whatsapp: +60165833302
Email: smitaobgyn@gmail.com


Why Us?
About Us
Services
Endometriosis
Robotic Surgery
Articles